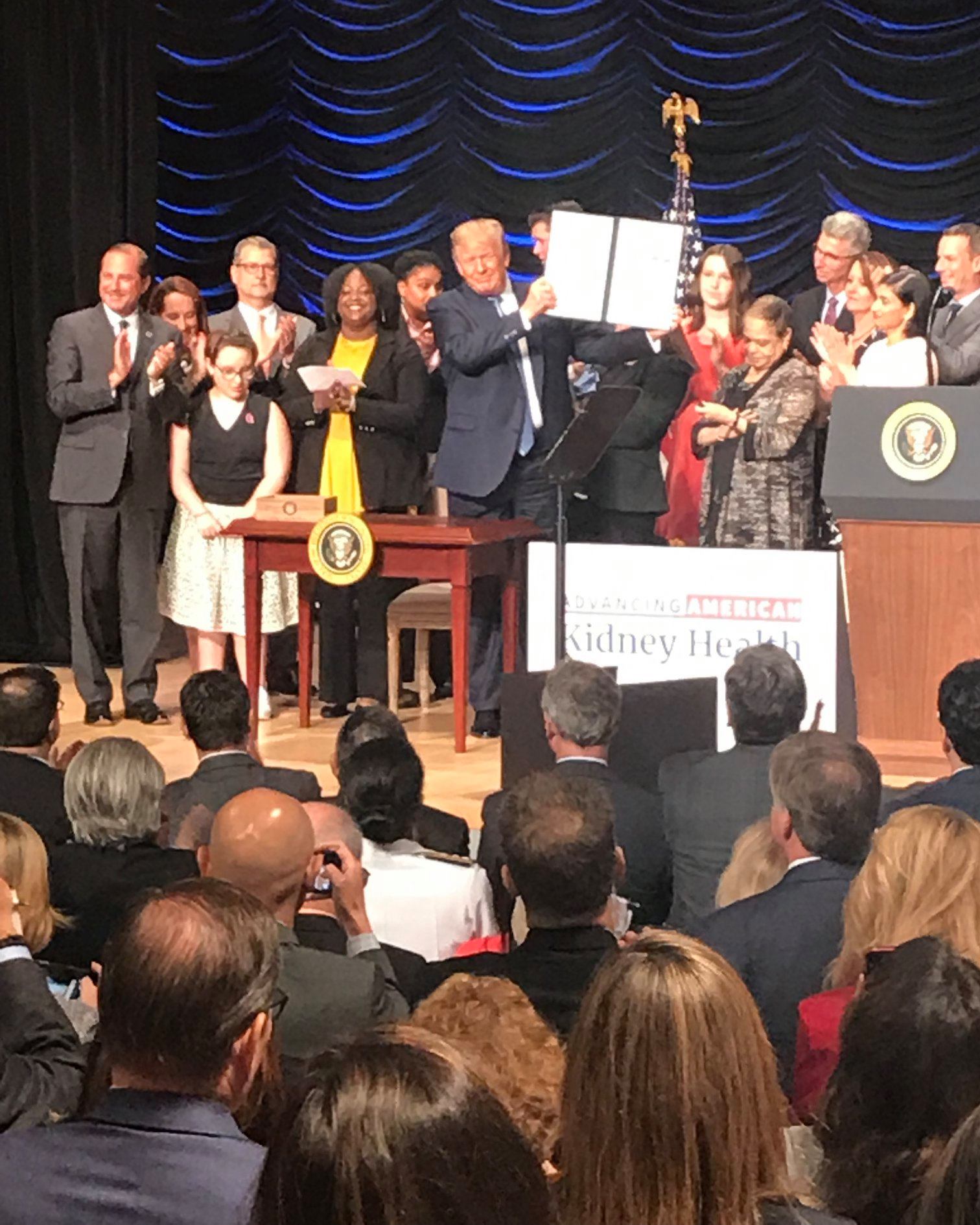
Last Wednesday, Director of Government Affairs Alexis Denny attended the signing of an executive order titled Advancing American Kidney Health. This order and its accompanying policies mark one of few times a sitting president has brought chronic kidney disease — and the obstacles this community faces — to the forefront. We encourage our community to read the order and other articles about it:
- Politico Article: Trump Aims to Shake Up Kidney Care
- NPR All Things Considered: Trump Administration Announces Plans To Shake Up The Kidney Care Industry
- NPR Weekend Edition Story: Overhauling Kidney Care
- Visual representation of the executive order
Read on for Alexis’s take on how the PKD Foundation views the program, how it will impact PKD patients in the U.S., and what the next steps for our community are.
PKD Foundation staff in D.C.
The PKD Foundation had strong representation at the event. I was joined by our CEO Andy Betts, board members Ashley Brown and Bill Brazell, and patient advocates Mary Ann Brazell, Meg Munits, and her son Dov Munits. “It was an exciting day for PKD and all kidney patients in the U.S., and it was great to have such a passionate group of PKD advocates in attendance. We look forward to the changes the new plan will bring, and we will be there every step of the way to ensure the PKD patient voice and experience are part of the conversation,” said Andy Betts.
See a slideshow of photos from the event on our Facebook page.
What does the executive order address?
In summary, the executive order (EO) addresses issues in kidney care from three main areas:
- Prevention and Dialysis
- Transplant and Living Donation
- Innovation in Treatment
Prevention and Dialysis
Current policy Does not support or incentivize early detection and prevention of chronic kidney disease (CKD). Instead, it is built to wait until kidney failure, and then send the vast majority of patients to a center for dialysis. Physicians are not well-trained to educate and support patients for do at-home dialysis, and often individuals do not even know they are in kidney failure until dialysis is required.
Executive order Calls for an awareness campaign to educate patients about kidney disease in the hopes of driving earlier diagnosis and prevention efforts, and for a new payment model to increase incentives for home dialysis and transplants with a goal of 80% of end-stage renal disease (ESRD) patients receiving either home dialysis or transplantation by 2025.
PKD impact Most people with PKD are aware of the disease long before they are in late stage kidney failure (if this was not your experience, please tell us your story in the comments). While we don’t know exactly how many PKD patients who are dialyzing are doing so at home, my experience based on conversations with a variety of patients and providers is that it is at a similar or possibly slightly higher rate than the general CKD population. Unfortunately, hard data to back this up are not available. Incentives for better patient education and increased patient choice are always welcome, but implementation details need to be spelled out. While home dialysis may be beneficial, there are larger issues to consider when pushing this option. Home dialysis will have unique issues; fortunately, we can look to the many other countries that use this in the majority of their dialysis cases to identify potential pitfalls and plan for them.
My initial questions include:
- What about individuals who do not live in a home large enough to house the equipment needed for home dialysis?
- What about those who live alone (home dialysis requires someone be trained to administer to the patient) or who live with someone not able to manage the dialysis machinery or manage unexpected issues?
Ensuring the incentives for patient choice are in place so that each person can make an informed and educated decision about the modality and location of dialysis that is right for them will be critical to the success of this new plan.
Transplant and Living Donation
Current policy We know that the waiting time for a kidney transplant is long; for years, the shortage of available kidneys at any given time has been around 100,000. This is due, in part, to inefficiency in Organ Procurement Organizations (OPOs). Additionally, living donors often pay expenses out of pocket to donate, have to take time off work for recovery, and may face future issues securing life, disability, or long-term care insurance.
Executive order Calls for testing of a new payment model based on cost and quality outcomes and focuses on delaying or preventing the onset of kidney failure, preventing unnecessary hospitalizations, and increasing rate of transplants. The order also calls for regulation of the OPOs to establish rules and evaluation metrics to increase transparency and efficiency, with intent to increase the number of kidneys (and other organs) available for transplant. Finally, it calls for new regulation to lower barriers to living donation. This regulation will increase a donor’s income limit eligible for reimbursement of expenses and expand allowable reimbursements to living donors to include lost wages and child and elder care. These expenses are reimbursed to eligible donors through the National Living Donor Assistance Center (NLDAC).
PKD Impact This portion of the order may be the most beneficial to PKD patients. Increased efficiency in OPOs in recovering more organs for transplants means more transplants, some of which will go to individuals with PKD. PKD patients tend to do better with transplants than general CKD patients, making it the desired option for our community.
Living donor support is exciting because many members of our community track their kidney function closely and know for months or even years they will eventually need a transplant. This means that PKD patients are well-situated to find living donors. Reducing barriers to living donation will increase the potential pool of donors and improve the odds of finding a donor.
Innovation in Treatment
Current policy Innovation in kidney care is something we don’t often hear about. The approaches to kidney failure have remained the same for much of the last 30+ years. Dialysis has been essentially the same since the 1970s and drug development has been largely focused on dialysis and transplant medications. Tolvaptan, the first approved drug to treat ADPKD in the US, was approved in April 2018 and is one of few medications ever approved to treat the cause of kidney disease.
Executive order Calls for investment in development of a wearable or implantable artificial kidney as well as investment in the Kidney Innovation Accelerator (KidneyX), a public-private partnership between the Department of Health and Human Services (HHS) and the American Society of Nephrology (ASN).
PKD Impact I admit to having conflicting feelings about this section. Development of a wearable or artificial kidney is long overdue and I applaud the Administration’s effort to drive that innovation. However, I am disappointed that nothing in the EO dedicates resources to therapy development efforts to prevent kidney failure from occurring in the first place. Singularly focusing on improving renal replacement therapy and transplant efficiency somewhat misses the mark for the PKD community (and other genetic kidney disease communities) by providing no pathway to increased funding of basic and clinical research to develop more and better therapies to stop the disease before it destroys the kidney. The PKD Foundation will continue to advocate for NIH funding to support basic and clinical science.
Final thoughts
As with most things in life (and government), the details will make or break this new plan. It is one thing to talk about big, sweeping changes to decades-old policy and to offer high-level ideals about ways to improve kidney care in the United States; it is another thing entirely to put those ideals into action, adjust when things don’t go as planned, and stay focused on the overall purpose: to improve the lives of everyone impacted by chronic kidney disease. The implementation details are not clear right now, and only time will tell us if these new policies will result in the intended outcomes.
This is the beginning, not the end, of the conversation. We have gained traction with this Administration, but we must also hold it accountable for the promises it has made. In his speech on Wednesday, the president stated that he will protect patients with preexisting conditions, and that his party agrees to do this as well. Signing this executive order is a step in the right direction, but we must also step back and not lose sight of the bigger picture. One that ensures patients have affordable access to the current and future therapies for PKD; that no one ever loses a kidney transplant because they cannot afford their immunosuppressive medications; that all patients have access to quality, affordable medical care; and that money for basic and medical research is increased year-over-year.
The PKD Foundation has your back — we will continue to fight for all of these things and hold the Administration accountable to make good on the promises it has made. We will continue to work closely with other kidney organizations to push as a community to truly and finally improve care for all PKD and kidney patients.
What do you think about the executive order? Tell us in the comments below!
Want to get involved?
- Check out the advocacy portion of our website.
- Sign up for Advocacy Alerts.
- Follow us on Twitter: @adennyPKD and @PKDFoundation
- Use our tools to tell Congress that you expect action!









I think continued work really needs to focus on providing donors health insurance for life. When people donate, many don’t realize they now have a pre-existing condition. This should not ever be a factor in someone not donating, ie fearing they will lose health insurance coverage. Actually, nobody should fear this. People are born with PKD or PPD. or other inherited diseases. I appreciate the PKD Foundation being advocates for people like me who inherited such a disease that affects not only the kidneys but extends to many other bodily systems as well.
Do we know when these orders take affect? Immediately? I’m wondering specifically about reimbursement for living donors. I may need a transplant as soon as this fall; will my living donor possibly be eligible for more benefits by then?
For such good news this effort is for pkd patients, this seems to be a skeptical view. Shouldn’t now be the time to praise the actions taken instead of almost assuming there will be no follow through? Would you have rather the president done like others and do nothing? This is an executive order with time-frames for action to help those with kidney issues. Sure, more could always be done. But for me, I am thankful and surprised this is being addressed in such a positive way. Not a time for skepticism or possibly slanted political views (see news links chosen). Thank you President Trump!
Hi Jennifer,
Thank you for your question! The timelines in the executive order are relatively quick, however as with any new policy, it does take a bit of time to make it happen. Part of the process for the living donor support specifically is to ensure the funding is appropriated in the budget. That is still in process for the next fiscal year (starts on October 1), so we are working to ensure the funding is included in that budget.
I am on dialysis at a center near my house. I am 83 years old and could not possibly do this at home. I have been advised of this option and decided not to do it. I also have no room for all the equipment needed. But for people who are still working I can see how it would work.
Thank you for sharing your experience Madeline!
my husband was diagnosed with PKD at age 61. He is currently 64 and Kidney output is 7%. He is about to be trained on Peritoneal Dialysis – after healing from surgery installing the Cath. We are currently in a living situation that can house the amount of equipment/supplies needed, but will expect a move in the near future and are concerned about how to properly store everything. We currently are on the look for a live donor. He is on a transplant list with a wait time of 3-4 years. My husband is very interested in the research being done on artificial kidneys, stem cell research, and studies being done at larger hospitals. While this is a genetic disease, he is the first in his family to have it diagnosed.
Thank you for sharing your experience Carolyn
I don’t trust the trump administration. It isn’t about improving our lives. Eventually, it’ll be about eliminating the need to spend federal dollars. We’ve been hornswoggled.
I have two sons who are waiting for kidneys. One is on dialysis and and has been trained in using equipment at home. I would like to see more doctors going into research to see what can be done to stop the eroding of the kidneys. It breaks my heart to know there is a 50/50 chance that my grandchildren will also have this horrible disease and there is no cure ! I know there are brilliant research doctors and I pray that God would lead them to a find a cure for so many desperate people waiting for a life !
Bless the many who donate a kidney so others may live. I personally feel that stem cell research may be the answer……I pray for an answer soon and pray my grandchildren do NOT have to go through what my sons are experiencing .
It would have been much better if the executive order also added that everyone in the US is automatically in an opt-in program as a deceased donor as many other countries have already done. This would have significantly increased the number of donations and lives changed and saved.
I am currently on peritoneal dialysis at home, and it is a very good option for me. However, finding a kidney has been much harder, I’ve been on the list for 5.5 years. I agree with the comment above about people having to opt out of being a donor instead of opting in. It would create a larger pool. I’m also concerned about the big business that is dialysis, mainly conducted by to major groups. While I don’t agree with the current administration on many things, this seems like a very good initiative. Although I’m sure it’s really about saving money, not saving lives. Time will tell, let’s stay vigilant!
I was unaware I had PKD until I was 48 & preparing for surgery. The surgeon saw my creatine raise with each lab report & advised me to the nephrologist immediately. I knew before I was even tested that I too, had inherited this disease. 3 out of 6 children in our family have PKD & for each of us, it only took 1 1/2 – 2 years to go from diagnoses to failure. I have been on the transplant list for 9 years, and pray that this is my year for one. I was recommended to do home dialysis but didn’t have anyone around nor the space for the supplies to make that option feasible. It is very discouraging to be in a dialysis unit for that long & rarely see a chair empty because the patient received a transplant, the chair is empty because the patient passed away
Descriptive information about transplantation and donor services! Thank you for updating me with such useful blogs.
Can PKDcure draft an email thanking the President and urging him to increase funding for research and ways to allow patients affordable access? It can then be posted on this site and submitted by many.