With a rigorous peer-review process and a commitment to funding the most promising scientific endeavors, the PKD Foundation grants empower researchers to make meaningful strides in the fight against PKD. Whether you're a seasoned investigator or a budding researcher, we invite you to explore our grant opportunities and join us in our mission to improve the lives of those affected by PKD.
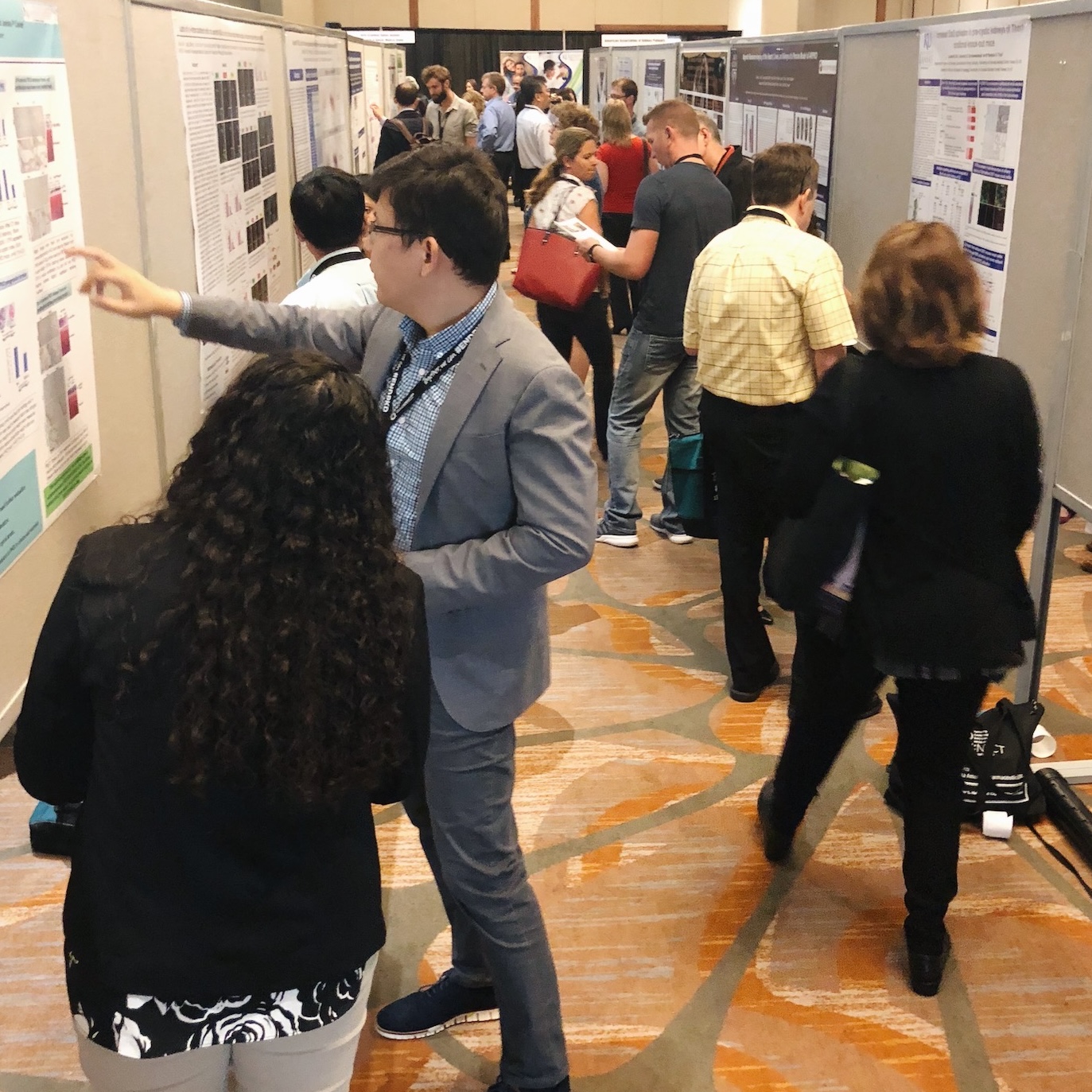
These grants aim to advance knowledge about the causes, progression, and potential treatments for PKD by funding research projects conducted by scientists, clinicians, and institutions worldwide. PKD research grants typically cover various expenses associated with the research, including personnel salaries, laboratory supplies, equipment, and other research-related costs. Through these grants, researchers are empowered to explore innovative ideas, conduct experiments, and generate data that contribute to the collective understanding of PKD and ultimately improve patient care and outcomes.
For designated PKD Centers of Excellence, Partner Clinics, Pediatric Centers of Excellence, or Pediatric Partner Clinics, care team grants may be used to support a wide range of activities, including the development of multidisciplinary clinics, patient education materials, support groups, and research into innovative care models. By fostering collaboration and innovation within the healthcare community, PKD care team grants seek to improve outcomes and quality of life for individuals living with PKD.

Open to PKD Centers of Excellence, Partner Clinics, Pediatric Centers of Excellence, or Pediatric Partner Clinics, community engagement grants may support a wide range of activities, including hosting educational workshops, organizing support groups, raising awareness through social media campaigns, and facilitating outreach efforts to underserved populations. By supporting community-driven initiatives, PKD community engagement grants aim to strengthen connections, amplify voices, and mobilize action within the PKD community, ultimately improving the lives of those affected by the disease.

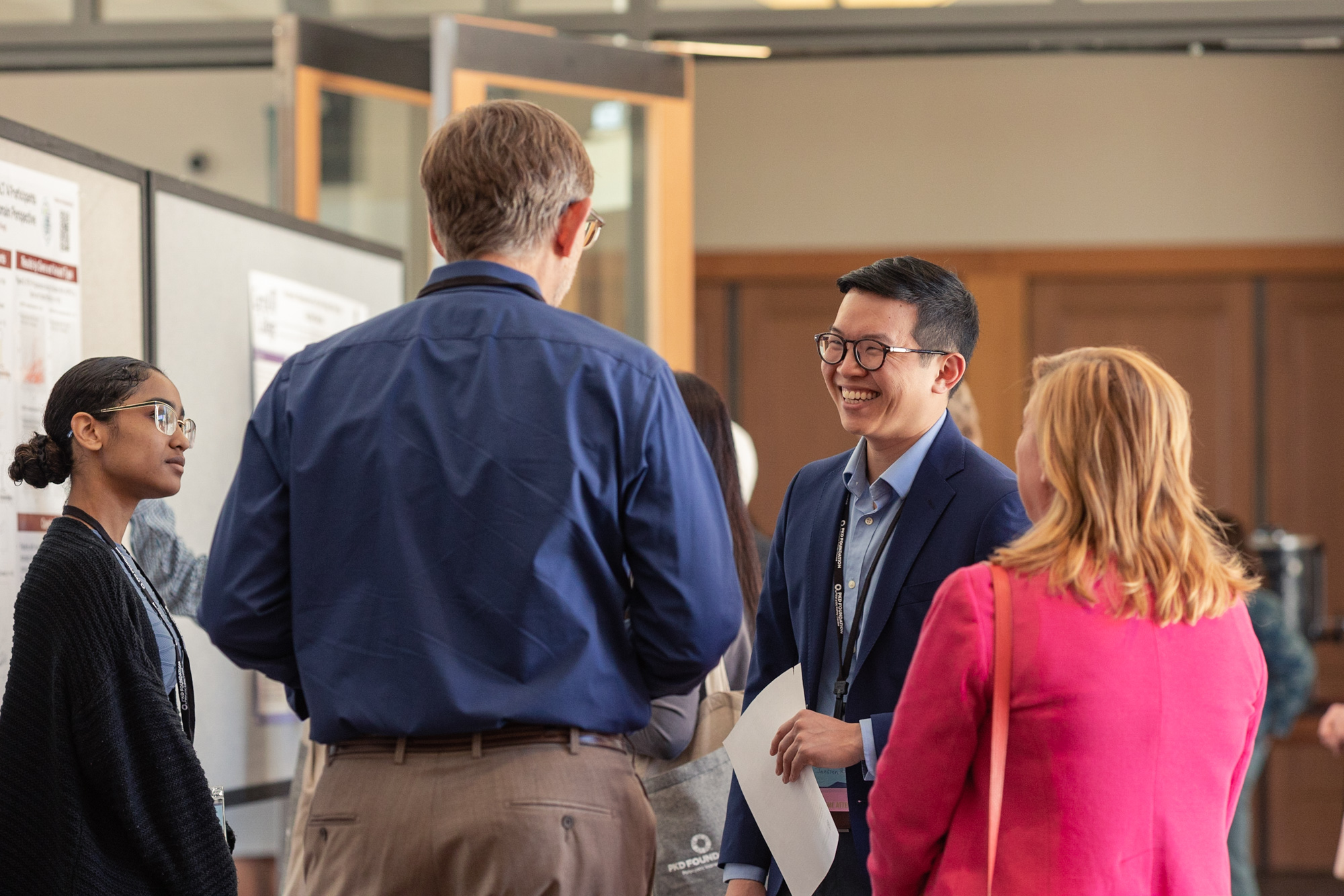
In 2024, we awarded new research funding to 13 outstanding PKD researchers. The goal of the Research Grant and Fellowship Programs are to fund critical research to increase understanding of the genetic and pathological processes involved in PKD and accelerate the development of potential therapies for PKD patients.
The review process
The Review Committee is comprised of the PKD Foundation Scientific Advisory Panel (SAP), additional ad hoc scientists and experts in PKD, as well as a Stakeholder Review Panel made up of PKD patients and caregivers. Each application is assigned three independent reviewers who rank the grants based on our Guidance for Reviewers that provide separate criteria for scientists and stakeholders. Read more about our Peer Review Process here.
Rankings are based on:
- significance to PKD research
- innovation
- investigator strengths
- scientific environment
- approach


- 2023
- ADPKD
- PKD
- PKDCON
- Research
- Webinar

- 2023
- ADPKD
- Diet
- Nutrition
- PKDCON
- Research
- Webinar

- 2023
- ADPKD
- Diet
- Nutrition
- PKDCON
- Research
- Webinar

- ADPKD
- Centers of Excellence
- Education
- Family Life
- PKD News
- PKD Parents
- Research

- ADPKD
- ARPKD
- Caregivers
- Education
- Living with PKD
- Newly Diagnosed
- Research
- The Basics of PKD

- ARPKD
- Family Life
- PKD Parents
- Research
- Young Children