Published on May 17, 2022 | Each year, tens of thousands of patients need organ transplants. However, the supply of available organs is much smaller than the demand. In order to combat the tremendous shortage of organs available for transplantation, researchers are working on a non-human solution. Recently, there’s been progress by generating pigs suitable to support pig-to-human organ transplants. A process called xenotransplantation.
The Basics of Xenotransplantation
What is it?
In short, xenotransplantation is grafting organs from animals into people.
Why do we need it?
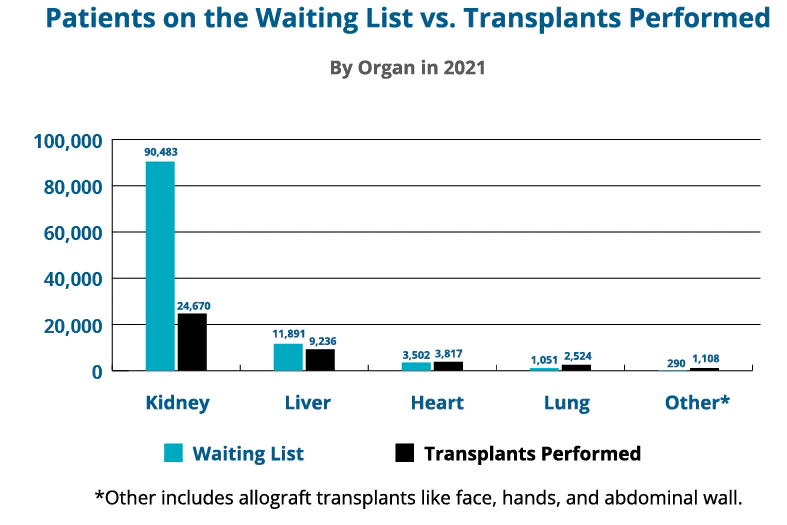
Statistics provided by organdonor.gov.
In 2021, there were 90,483 people on the kidney transplant waiting list. But according to the Health Resources & Services Administration, only 26,470 kidney transplants were performed (less than one third). Furthermore, they note that approximately 106,000 people in the US are on the organ donation waiting list—83% of whom are waiting for a kidney transplant. There’s a huge gap between organs needed and organ availability.
So, how do we approach filling the organ gap? One approach is xenotransplantation. In the last nine months, there have been four examples of xenotransplantation of organs from pigs to humans. Three separate kidney studies and one heart study. These represent the first ever examples of xenotransplantation of pig organs.
The History of Xenotransplantation
Research to understand the barriers of using xenotransplantation to address the human donor organs shortage has a long history. It can actually be traced back to the early 1900’s. By the early 1960’s, prior to the development of dialysis and the development of processes for obtaining deceased donor organs, several chimpanzee-to-human kidney transplants were attempted. Additionally, baboon-to-human kidney, heart, and liver transplants, were attempted. At the time, physician scientists expected that kidneys from closely related, nonhuman sources would respond similarly to human kidneys following transplantation into humans.
Given challenges and ethical concerns associated with using primates for this research, efforts transitioned to evaluating pigs as donor animals.
So, Why Pigs?
Since the 1990’s, pigs have been the animal of choice for xenotransplantation research for several reasons:
- Pig organs (particularly kidney and heart) function very similarly to human kidneys and hearts.
- In terms of kidneys, the kidney function measures in pigs and humans are very similar.
- Their organs are similar in size to humans.
- Pigs have a long life expectancy (~30 years). Meaning there’s hope that a pig-to-human transplant would be long-lived in the human recipient.
- Pigs reproduce relatively rapidly and have a large litter size providing the potential to produce a large supply of organs (eg. pigs are a scalable species to produce donor organs).
- They can be raised in environments free from pathogens (eg. viruses or bacteria that could potentially infect humans). This prevents the risk of transferring pig viruses into the recipient.
Overcoming Barriers
In order to make xenotransplantation viable, we need to overcome several barriers. The first major barrier is that after transplantation of the pig organ, our immune system rapidly recognizes the organ as foreign and attacks it. This leads to immediate (eg. acute) rejection. Secondly, if drugs are used to suppress the immune response, the cells that line the blood vessels of the pig organ lack the factors needed to keep human blood from clotting within them. This causes blood clots to form within the donated organ leading to organ death.
Over the last 30+ years, researchers worked to find solutions to these barriers. Through research they identified:
- Critical factors on the pig organs recognized by the human immune system that lead to acute rejection
- Missing factors from the pig organs to maintain flow of human blood through the pig organ;
- Factors present in our tissues that help prevent our immune systems from attacking self
All these advances were necessary to define what would be needed for a pig organ to potentially survive in a human. However, scientists still needed to be able to engineer pigs with all necessary genetic changes from which one could obtain organs potentially suitable for xenotransplantation.
Genes and Xenotransplantation
Until recently, the tools to extensively genetically engineer pigs to make the necessary changes weren’t available. Gene editing technology has advanced to enable scientists to make substantial changes to pig genome. Therefor, making genetically engineering pigs potentially suitable for xenotransplantation. Scientists engineered pigs to produce organs compatible with the human immune and blood clotting systems. This is often called the “10-gene pig” in the news.
So, what does that mean? They removed genes from pigs that make the pig organs less pig-like to make them more human like. In the examples of pig-to-human kidney transplants, 10 genetic changes were made in the pigs. Three genes were removed from the pig that would trigger the human immune system and cause immediate rejection. Accordingly, a fourth gene was removed to prevent the pig organ from growing too large after transplantation. Altogether, six human genes were added to the pig to prevent the recipient’s immune system from attacking the organ and to prevent blood clots from forming in the organ.
Recent Experiments of Xenotransplantation
Extensive testing has been done on genetically modified pig kidneys in pig-to-primate transplant studies. However, it’s a big jump to go from transplanting pig organs in primates to transplanting pig organs into humans. Importantly, there have been several medical interventions that looked promising in primates but had a different response in humans.
So, before proceeding to clinical studies, researchers conducted an intermediate experiment to obtain data in a human system without risking the life of a patient. Through consultation with ethicists, researchers decided that performing xenotransplants in brain-dead individuals (on life-support) would be an appropriate approach to understanding if pig-to-human kidney transplant is feasible. The same qualifying factors in identifying a deceased organ donor candidate were used in these studies. However, once a family consented to allowing their family member to participate, they could no longer qualify as a deceased donor in the future.
Thank you to the families who donated a loved one for these experiments. Because of you, incredible advancements in science were made possible.
Milestones in Kidney Xenotransplantation
At NYU Langone Health, a surgical team wanted to evaluate if an organ from a 10-gene pig would be protected from acute rejection and clot formation when attached to a brain-dead person on life support. Twice they attached a pig kidney to blood vessels in the thigh of the person to monitor survival of the organ and sample the tissue. Their goal was to understand how it responds to exposure to the human system.
Both experiments were successful. The organ survived and didn’t show signs of rejection through the planned 54-hour follow-up period and produced urine demonstrating the kidney functioned.
At the University of Alabama, Birmingham, a surgical team wanted to evaluate if the tests they developed to properly cross-match a pig organ with a human recipient worked. Cross-matching is the donor matching process used to determine if a donor and patient are a suitable match. This resulted in the first pig-to-human kidney transplant.
They transplanted two kidneys obtained from a 10-gene pig into a brain-dead recipient on life support. Replicating the full clinical transplant process, the pig organs replaced the deceased organ donor. Much like the other experiment, this resulted in another success—the organ survived. Through the three day, follow-up period, it showed no signs of rejection and produced urine demonstrating the kidney functioned.
The success of both studies is a major milestone in the field of transplantation. Studies like these bridge critical knowledge gaps and obtain safety/feasibility data to support a clinical trial in humans with kidney failure. With their findings, xenotransplantation advances as a potential approach to filling the organ shortage gap.
What’s Next?
In conclusion, it’s likely that more experiments like these will be conducted to provide additional feasibility and safety data, closing the remaining gaps in knowledge before moving to clinical studies. There will need to be significant collaboration between research teams and the FDA. First, they’ll need to determine if enough is known to move to living people. Secondly, they’ll need to develop appropriate study protocols.
For example, how should patients be selected for such trials? What needs to be done to properly protect a patient who participates in such a study?
The research teams that conducted these studies hope to transition to clinical studies in living patients in 1-2 years. As these studies progress, the path to faster transplantation becomes more likely.
Interested in reading transplant stories from the PKD community? Check out this blog from National Donate Life month.









This would be a game changer. How do you sign up for trials?
The research teams that conducted these studies hope to transition to clinical studies in living patients in 1-2 years. You can find clinical studies that are currently enrolling here: https://clinicalstudies.pkdcure.org
Very interesting read! While still in its early phases, xenotransplantation has the potential to save the lives of those suffering from severe cardiac disease and renal failure. Experiments using transplanted pig cells in Parkinson’s and diabetes patients have yielded promising preliminary results. Furthermore, if the barriers are overcome, xenotransplantation may provide patients needing an organ transplant with a faster, less expensive, and more efficient option.
My brother died of kidney failure and if he would have had a chance to live even with a pig kidney. I think he would have joined I hope this can help Others that are suffering from Kidney failure if he would have been able to join this program it at least would have given him. Some type of hope and maybe live a little longer. I hope this program can help others not go through the pain that my family and I have went through. I have lost siblings because they needed donors donuts and couldn’t find them after losing my 1st brother I decided to become a donor on my license. I have a lot of rare diseases but I still want to be a donor in science. To help other people not go through what my family has went through and losing 5 siblings. There are only 2 of us left now. And I support any program that can help family members not go through the problems that I have went through. My family has went through because we have rare mutations in our body organs that don’t wanna work properly rare cancers that only one in the billion May. Get blood clot disorders that 1 and a billion May get. I hope this can help other people not go through the pain that my family went to
I remember when Dr. Barnard did the first heart transplant. It was huge news. I was a kid so I didn’t understand the impact it would have in years and patients to come. Hopefully this work toward pigs’ hearts for human transplants may become viable and another piece of history.